In This Issue
The opinions, beliefs and viewpoints expressed in this publication are those of the authors. They do not necessarily reflect the opinions, beliefs, viewpoints or official policies of Autism Society Alberta.
|
|
|
End article-->
Autism Alberta's Family Resource Centres
Click the poster below to see a larger version
Click here to learn more about the Family Resource Centres
|
|
|
End article-->
Autism Alberta's Summer Support Group Meetings

As part of Autism Alberta's Family Resource Centres, our Family Resource Coordinators are hosting a new series of support group meetings.
For more information about any of the upcoming meetings, you can contact our Family Resource Coordinators at FamilyResourceCentres@autismalberta.ca or 587-282-1424.
Thursday, July 8th - 7:00pm
Google Meet joining info
Video call link: https://meet.google.com/rqy-dczi-kaa
Or dial: (CA) +1 226-317-6906 PIN: 500 411 987#
More phone numbers: https://tel.meet/rqy-dczi-kaa?pin=3261910529446
Tuesday, July 20th - 1:30pm
Google Meet joining info
Video call link: meet.google.com/jns-hdcp-ndh
Or dial: (CA) +1 289-949-6639 PIN: 739 433 112#
More phone numbers: https://tel.meet/jns-hdcp-ndh?pin=7336068210224&hs=0
|
|
|
End article-->
Self-Care Milestones and How We Got There
Kitty Parlby
Recently I posted a short video of our 24-year-old autistic son Eric shaving independently, saying how proud I am of him. Today I’m going to talk about shaving, showering and tooth brushing. Some of these strategies will be applicable to any age.
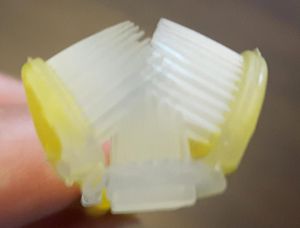
When he was 15, we began shaving him. We started to get him to practice, and in about 3 weeks he was doing it by himself. But after shaving independently for a month or so, we found that he was still cutting himself too much. This was partly due to motor skills, but mostly due to the rigidity and  patterns that come with Eric’s autism. We had to transition him to an electric razor; however, Eric’s biggest sensory issue is tactile. So we periodically tried different electric razors, often 6 months or more apart. This time, I researched razors that were quieter, with less vibration. I also decided to start with a wet/dry shaver (the Panasonic ES-LV95-S 5-Blade Wet/Dry Shaver, to be exact). And indeed, for the first 3 weeks, Eric did use his new shaver with shaving cream until he got used to the sound and feel of it. Then one day I said, “You know, it would take less time to shave and clean up if you used it without shaving cream.” Boom! Done! Our success was partly due to strategies, but it was also because he himself was ready. patterns that come with Eric’s autism. We had to transition him to an electric razor; however, Eric’s biggest sensory issue is tactile. So we periodically tried different electric razors, often 6 months or more apart. This time, I researched razors that were quieter, with less vibration. I also decided to start with a wet/dry shaver (the Panasonic ES-LV95-S 5-Blade Wet/Dry Shaver, to be exact). And indeed, for the first 3 weeks, Eric did use his new shaver with shaving cream until he got used to the sound and feel of it. Then one day I said, “You know, it would take less time to shave and clean up if you used it without shaving cream.” Boom! Done! Our success was partly due to strategies, but it was also because he himself was ready.
Likewise, moving Eric from baths to showers in his teens took a full year of strategy. With his tactile defensive issues, he loved being submerged in water – it’s like a deep hug – but water droplets falling on him is light touch. We used a shower assembly that includes a ‘rain shower’ head, which feels different than a typical shower head, and a hand wand attachment. That gave him options. I also taught him how to adjust the rate of water flow and the temperature. Brushing his teeth was a long haul, too. What ended up working for him was a manual 3-sided toothbrush, which made the job much quicker. No electric toothbrush for him, as the vibration inside his mouth was just too much.
 So let’s get into strategies that are applicable for self-care skills. I have used most of these with Eric. These ideas may also be helpful for many other challenges and goals: So let’s get into strategies that are applicable for self-care skills. I have used most of these with Eric. These ideas may also be helpful for many other challenges and goals:
-
Model and comment. Whatever skill they’re working on, make sure they get a chance to see others doing it on a regular basis. During and after, have the person modelling comment about it. Over time, this can gradually get your autistic family member used to the benefits and reasons for the skill, and provide clues on how it feels. Here are some examples of effective commenting while modelling shaving: “I like the feeling/smell of this shaving cream.” “My skin is nice and smooth now, not rough and stubbly.” “Wow, I look and feel much better!” “My electric razor does a great job. It’s easy to use and I don’t even have to use shaving cream.” “It’s a hot day, but my face will feel much cooler now that I’ve shaved.” This kind of situational commenting can be used for any skill, and doesn’t exert pressure on the watcher.
-
Engage the senses of the person you’re modelling for. If you’re working on transitioning to showers, offer to let them smell the soap/shampoo/conditioner you’ll be using; if you have more than one choice, ask which they think you should use. Use the bathroom sink and run the taps, experimenting with the temperature, and ask what they think would be a good temperature for your shower. Let them do an activity in the bathroom while you are showering, so they can experience the increased humidity and how it sounds. Let them write/draw in the steam on your mirror. Ask them to help comb your hair afterwards. This, in essence, is exposure therapy – exposing them to the environment. You can often adapt this to decrease any sensory discomfort for them. Of course, when needed, you can reach for a towel, dry in the shower, and cover up before you step out.
-
When out and about, the whole family should be in the habit of describing how they are feeling in regards to the skills being targeted. Here are some examples: “I’m so sweaty after our hike; a shower would  feel really good.” “Those caramels taste great, but some of it is stuck between my teeth. I need to brush.” “I love hugs from your dad, but his whiskers are scratching my cheek. He needs a shave.” “I need to go to the bathroom. Where’s the nearest one?” Basically, you’re voicing the benefits of the skill you are aiming for. feel really good.” “Those caramels taste great, but some of it is stuck between my teeth. I need to brush.” “I love hugs from your dad, but his whiskers are scratching my cheek. He needs a shave.” “I need to go to the bathroom. Where’s the nearest one?” Basically, you’re voicing the benefits of the skill you are aiming for.
Of course, there are many more direct strategies, such as giving choices, offering rewards, social stories, graduated exposure, making a game of it, etc. You don’t want to be forceful, especially around self-care skills like toileting, eating, bathing/showering, shaving and brushing teeth. You don’t want them to have negative feelings about these skills and shy away from them even more. If your strategy is unsuccessful, you may need to wait a while before trying something else. Trial and error, patience, and humour are some of your most valuable tools.
Remember, it’s their body. Accept that they may take longer than typical to see the value of the skill, or to develop the ability to withstand the sensory issues. Train yourself to wait a few minutes before doing it for them, to see if they may one day surprise you. When picking what to work on, get their input, and choose what will make the most positive impact on their life. Most of all, keep in mind there is no age limit to gaining a skill. When you least expect it, you will be like me, the proud parent sharing her son’s shaving triumph!
Kitty Parlby is the mother of an autistic young adult. She is a former special needs Educational Assistant and an autism speaker and consultant with Autism Inspirations. She currently works as a Family Resource Coordinator for Autism Society Alberta.
|
|
|
Defining the Spectrum
Nicole Burnett
When viewing autism from a diagnostic perspective, everyone is gauged by the same metric – the DSM-V criteria – which does not demonstrate the vast diversity among individuals. The DSM uses a categorical system – the criteria are met for a disorder, or they are not. Someone meets the criteria for Autism Spectrum Disorder, or they do not. The system does not have a gray area. The diagnosis of autism itself is best described as “box checking”: a behaviour is present, or not. However, how that behaviour manifests itself may be different across individuals. For example, the criteria of “communication difficulties” could mean many things, such as being non- verbal or using atypical conversational rules. These differences in the expression of behaviours are what define autism as a Spectrum Disorder and account for the variability across individuals. You have probably heard the Stephen Shore quote, “If you’ve met one person with autism, you’ve met one person with autism.” This statement reflects the fact that there are individual differences in the Spectrum, and a diagnosis is not a one-size-fits-all definition. verbal or using atypical conversational rules. These differences in the expression of behaviours are what define autism as a Spectrum Disorder and account for the variability across individuals. You have probably heard the Stephen Shore quote, “If you’ve met one person with autism, you’ve met one person with autism.” This statement reflects the fact that there are individual differences in the Spectrum, and a diagnosis is not a one-size-fits-all definition.
A common analogy used to describe the spectrum is a comparison to the colour wheel. All the colours are present, whether they appear in the rainbow or not. Which colour is visible in the rainbow depends on the observer and the environmental conditions. Apply this notion to the autism spectrum: all the behaviours are there, but the range of how those behaviours are demonstrated varies across individuals. It is also important to note that there may be differences in the expression of behaviours within the individual themselves, depending on the context or environment. For example, someone in a new environment may engage in more repetitive behaviours to soothe their anxieties, but in a familiar environment, they may not need to stim.
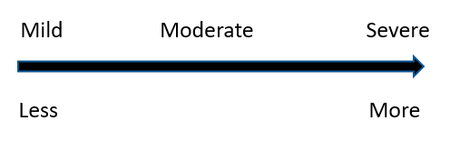
It is also important to note that the spectrum is often confused with a similar concept, that of a scale (depicted below). The scale was a popular tool used in the ‘80s, when autism was first introduced in DSM-III (Wing, 1988). This concept has hung on over the decades, but in modern times is wholly inappropriate. A scale implies that there can be more or less of a concept, and imposes terms like mild, moderate, and severe. Thus, someone with mild autism may be interpreted as “less autistic” when compared to someone with severe autism. The concept of a scale does not reflect ASD, as both of those individuals were diagnosed using the same diagnostic criteria. Someone cannot be more autistic than another. Another saying applies here: “different, not less.” The use of a scale has been discontinued, because it can lead to further stigma due to the social categorization that can result.
A new concept has been proposed to replace terminology of spectrum and scale, and instead refer to autism as a constellation (Fletcher-Watson & Happe, 2019). A constellation imagines autism as multidimensional and flexible. The constellation allows for the fluidity of behavioural expression, rather than a static description captured by a questionnaire or assessment in a file somewhere. This modern term may also help combat stigma that surrounds an ASD diagnosis. Regardless of the terminology, individuals with ASD have independent strengths, identities, and make important contributions to society.
Dr. Burnett is a professor of psychology at Medicine Hat College.
|
|
|
COVID-19 Disability Survey

Living with a Disability During COVID-19?
The COVID-19 Disability Survey is a special initiative to record the experiences, concerns and needs of people with disabilities during the COVID-19 outbreak and recovery period.
The survey’s findings will provide important information to help communities ensure that COVID-19 response strategies meet the needs of people of all abilities.
Click here to learn more and to take the survey
|
|
|
End article-->
Autism Insights – June 2021

Autism Calgary have released a new episode of Autism Insights, their video e-magazine! The latest episode features:
- A profile of Lyndon Parakin, Executive Director of Autism Calgary
- Fitness tips with Maureen Bennie
- Intro to our medical health team, Dr. Roger Thomas and son Bennett Thomas
- And Dr. Joel Christie gives sage advice about how to address social isolation
Click here to watch

|
|
|
End article-->
The Power of "Yet"
Karla Power
 Today is Paddy’s 6th birthday, and for some reason it feels like a big one! He has grown so much this year, in every way. As he moves out of the little boy phase and into becoming a big boy, we couldn’t be prouder! Today is Paddy’s 6th birthday, and for some reason it feels like a big one! He has grown so much this year, in every way. As he moves out of the little boy phase and into becoming a big boy, we couldn’t be prouder!
This also marks the last month of Kindergarten for Paddy. He will be moving into Grade 1 next year after three years in early years education, and after last week’s ISSP meeting, we feel he is ready.
Even though there have been many changes and bumps in the road – a change in EA, three isolations, and five weeks of online learning – Paddy has had a wonderful year! For the first time ever, we have seen the word “achieved” for several goals. I joked with the team that this may be my new favourite word, but I truly could not be prouder of this little dude!
What makes these accomplishments even more astounding is that, on paper, Paddy presents as “severe” and at or below the 1st percentile in almost every modality (speech and language, fine and gross motor). So, when Paddy began to make eye contact, interact with peers, hold a pencil, throw a ball, and use the washroom independently this year, it was cause for huge celebration!
As for the goals that were not accomplished, we all agreed that Paddy will be able to do these things, just not yet. When I think about the power of this word, it brings up lots of emotions. “Yet” gives us hope; it reminds us that Paddy is capable and needs to be gently pushed; it lets us dream of a future where anything is possible.
Paddy’s school team may not realize this, but they gave us a gift this year. When we were barely staying afloat as parents, being bogged down by teaching and parenting during a pandemic, they never let us give up on the  most important things in our lives: our boys! They led the way by gently pushing our amazing boy to do things we never thought possible. most important things in our lives: our boys! They led the way by gently pushing our amazing boy to do things we never thought possible.
Paddy’s team went above and beyond this year – not just for our son, but for our whole family! They truly are a “Dream Team” for believing in our boy and giving us the gift of “yet”. I can’t wait to see what this awesome 6-year-old will do next!
|
|
|
Estate Planning Series: Part 4 – Disability Tax Credit
Gergely Hegedus
Last month, in Part 3 of this series, we discussed the Qualified Disability Trust (QDT), as well as the criteria a testamentary trust must meet in order to qualify as a QDT. The article noted that in order for a testamentary trust to be designated as a QDT, the qualifying beneficiary of the trust must qualify for the Disability Tax Credit. In Part 4 of this series we are going to discuss the Disability Tax Credit, including a discussion of what it is and how an individual can qualify for it.
What is it?
The disability tax credit (DTC) is a non-refundable tax credit that helps persons with disabilities or their supporting persons reduce the amount of income tax they may have to pay.
 The DTC can open the door to other federal, provincial, or territorial programs such as the registered disability savings plan, the Canada workers benefit, and the child disability benefit. The DTC can open the door to other federal, provincial, or territorial programs such as the registered disability savings plan, the Canada workers benefit, and the child disability benefit.
How much is it?
In 2020, the maximum disability amount was $8,576, and the maximum supplement for persons under 18 was $5,003.
For whom can you claim the DTC?
You can claim the DTC for yourself, your dependent, or your spouse or common-law partner on your T1 Income Tax and Benefit Return.
What if I didn’t claim the DTC in the past?
If a person was eligible for the DTC for previous years but did not claim the disability amount when he or she sent his or her tax return, then they can request adjustments for up to 10 years under the CRA's Taxpayer Relief Provision.
How do I qualify?
To qualify for the DTC, you must meet one of the following criteria:
The BADL include the following: speaking, hearing, walking, eliminating (bowel or bladder functions), feeding, dressing, or performing the mental functions necessary for everyday life.
A person is markedly restricted if he or she is unable to do, or takes an inordinate amount of time to do, one or more of the basic activities of daily living, even with therapy
A person is significantly restricted if his or her ability to do a basic activity of daily living is still greatly restricted all or substantially all of the time (at least 90% of the time).
To qualify for the DTC, your impairment must meet all of the following criteria:
-
be prolonged, which means the impairment has lasted, or is expected to last, for a continuous period of at least 12 months
-
be present all or substantially all the time (at least 90% of the time)
What do I need to do?
 A medical practitioner has to fill out a form, certify that you have a severe and prolonged impairment, and must describe its effects. A medical practitioner has to fill out a form, certify that you have a severe and prolonged impairment, and must describe its effects.
Do people with autism spectrum disorder qualify?
The Tax Court of Canada has held that individuals who have autism spectrum disorder may be entitled to the DTC, as their ability to perform basic activities of daily living, including perceiving, thinking and remembering, may be markedly restricted.
Part Five of this estate planning series will discuss Registered Disability Savings Plans, and how you can incorporate these savings plans into your estate planning.
Gergely Hegedus
Partner, Tax Group at Dentons Canada LLP
For further information regarding the information contained in this article, you can reach Gergely at gergely.hegedus@dentons.com.
*Disclaimer – this estate planning series is provided as information only and may include items reported from other sources. The author does not warrant is accuracy. This information is not meant as a legal opinion or advice.
|
|
|
Improv Groups for Teens and Adults

STA is pleased to offer two 4-week theatre improv-based social skills groups, informed by principles of Cognitive Behavioural Therapy (CBT). The groups will support individuals with ASD ages 14 to 17 (Teen Group) and ages 18 to 24 (Young Adult Group) to practice social skills and manage social anxiety in a dynamic setting.
Who is it for?
Autistic teens and young adults who:
- Can discuss their thoughts, emotions, and experiences
- Are located in the province of Alberta
- Have access to technology that supports video conferencing
- Can commit to attending at least 3 out of 4 sessions
View the Young Adult Group poster
View the Teen Group poster
|
|
|
End article-->
Latest News from the Sinneave Family Foundation

Launch Into Life!
 The Launch into Life! QuickStart Planning Tool is a new, free, online resource that was created for adolescents and young adults who are interested in creating a personalized plan for their future. It will help you understand where you are now, what you want your adult life to look like, and what you need to do next to achieve your goals. The Launch into Life! QuickStart Planning Tool is a new, free, online resource that was created for adolescents and young adults who are interested in creating a personalized plan for their future. It will help you understand where you are now, what you want your adult life to look like, and what you need to do next to achieve your goals.
Read more
Summer 2021: EmploymentWorks Virtual
 This 4-week program is for neurodiverse individuals over the age of 15 who are motivated to find a job. This 4-week program is for neurodiverse individuals over the age of 15 who are motivated to find a job.
This free virtual program will give individuals access to structured learning and virtual job simulations. Employment Works Virtual starts this summer!
Read more
Click here to subscribe to the Sinneave Family Foundation newsletter
|
|
|
End article-->
What is a Sensory Diet?
Maureen Bennie

From the Autism Awareness Centre Inc. Blog:
 A sensory diet, first created by occupational therapists Wilbarger and Wilbarger (1991), is an individualized plan of physical activities and accommodations to help a person meet their sensory needs. This plan provides the sensory input needed to stay focused and organized throughout the day. For example, some people may feel overwhelmed or overloaded and need to get to a calmer state; some may feel lethargic or sluggish and need some activities to feel alert. A sensory diet, first created by occupational therapists Wilbarger and Wilbarger (1991), is an individualized plan of physical activities and accommodations to help a person meet their sensory needs. This plan provides the sensory input needed to stay focused and organized throughout the day. For example, some people may feel overwhelmed or overloaded and need to get to a calmer state; some may feel lethargic or sluggish and need some activities to feel alert.
The main goal of a sensory diet is to prevent sensory and emotional overload by meeting the nervous system’s sensory needs; however, it can also be used as a recovery technique. Understanding a child’s sensory profile and the activities which create calmness and regulation can really help when a child feels overwhelmed and out of control. Engaging children in sensory experiences on a regular schedule can support focus, attentiveness and interaction. Children may feel less anxious when they feel comfortable and in control.
An occupational therapist (OT) usually designs a sensory diet. Parents and caregivers can then use the tailored activities at home; teachers/educational assistants can use it at school. The reason it is recommended to consult with an OT who has experience with sensory processing issues is because one the trickiest aspects of sensory difficulty is recognizing when a child is overreactive or underreactive in any given moment, then adjusting sensory input to meet them where they are, and providing the right challenge to help them move forward into a “just right” state of being.
Observational checklists can be used to gather information about a person’s sensory profile. There are numerous sensory checklists available online or in books such as Answers to Questions Teachers Ask about Sensory Integration or Building Bridges Through Sensory Integration.
Activities for a Sensory Diet
Certain activities address specific sensory systems. Activities will also vary based on age and ability. Here are some examples of activities that can be used as part of a sensory diet:
Proprioception
Proprioceptive input can be achieved through lifting, pushing, and pulling heavy objects. Some ideas are:
- pushing a stroller or cart
- pulling a wagon filled with objects
- carrying a backpack
- playing hopscotch
- push-ups against the wall
 lifting weights lifting weights- wearing a weighted vest
- vacuuming
- swimming
Vestibular
Vestibular input (sense of movement) is created by any type of movement such as spinning or swinging. Some ideas are:
- swinging on a swing
- lying in a hammock
- spinning on a Sit 'n Spin or disc
- rolling
- jumping jacks
- dancing
Tactile
The tactile sense detects light touch, deep pressure, texture, temperature, vibration, and pain. Some ideas are:
- drawing in sand or salt
- hand massage
- high fives
- play with therapy putty, squeeze balls, or a band to pull on
- crocheting, knitting or sewing
- messy play with shaving cream or foamy soap
Auditory
Auditory input is what we hear and how we listen. Some ideas for calming and organizing auditory input are:
- listening to music
- listening to sounds in nature
- using noise-cancelling headphones to dampen sound
- playing a musical instrument
- listening to running water
Visual
Some environments can be too visually stimulating, such as classrooms with busy bulletin boards, brightly lit rooms, bright colors, or busy patterns on the wall or curtains. To reduce visual stimulation:
- keeps areas organized and clutter free
- store items in bins or boxes
- avoid using fluorescent lighting
- use neutral paint colors
Smell
Smelling certain odors can stimulate, calm, or send a person into sensory overload. When it comes to smells, think about:
- exploring calming scents to discover preferences. Lavender, vanilla, jasmine and rose are examples of calming scents.
 exploring alerting scents like peppermint or citrus exploring alerting scents like peppermint or citrus- sniffing different herbs and spices
- Some people don’t like scents at all. Look for unscented products such as detergents, soap or shampoo.
Taste
Taste input is perceived by the tongue, but how it’s interpreted or experienced is strongly influenced by the sense of smell. When it comes to taste, experiment with different flavors. Oral sensory processing not only involves taste, but the tactile and proprioceptive senses, too.
- Strong tastes can stimulate the undersensitive child.
- Involve children in food preparation to increase their likelihood of trying new foods.
- Offer crunchy foods such as raw veggies, popcorn, pretzels, or apples for those who like to chew.
- Other ideas for chewy foods are fruit leather, beef jerky, marshmallows or raisins.
- Children who like to chew can also use chewy jewelry.
- For children who like to suck or lick things, try popsicles, ice cubes, or drinking through a straw.
 These are just a few of the optional activities that can be used to created a sensory diet. To have a look at some examples, click here. Pinterest has lots of examples of sensory diets and templates. There are also some great printables organized by sensory system and age. Work with an experienced OT who can not only create a sensory diet, but also assist with visual supports and scheduling the activities throughout the day. These are just a few of the optional activities that can be used to created a sensory diet. To have a look at some examples, click here. Pinterest has lots of examples of sensory diets and templates. There are also some great printables organized by sensory system and age. Work with an experienced OT who can not only create a sensory diet, but also assist with visual supports and scheduling the activities throughout the day.
Ideas for classroom accommodations can be found here, and sensory diet activities for home here. Some resources to support teens and young adults are The Out-of-Sync Child Grows Up – Coping with Sensory Processing Disorder in the Adolescent and Young Adult Years and The Sensory Team Handbook.
If you are looking for ideas on how to support autistic adults with sensory issues, have a look at the book Sensory Issues for Adults with Autism Spectrum Disorder.
|
|
|
|
|